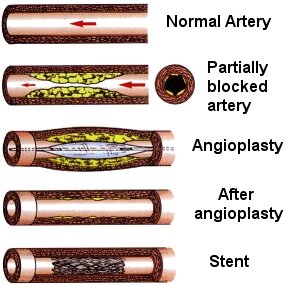
This is a treatment to improve the blood supply through the narrowed artery. It is know as a P.T.C.A. (Percutaneous Transluminal Coronary Angioplasty). It involves opening up the artery using a balloon.
How is the procedure performed?
This procedure is undertaken in the cardiac catheterisation laboratory using x-ray screening. The procedure involves passing a fine plastic tube (referred to as a sheath) into an artery via a small puncture hole in the groin or a small cut in the arm, under local anaesthetic. The groin is the usual site.
Through this sheath another fine tube called a guiding catheter is passed. This is threaded up to the heart and is positioned at the opening of the coronary artery. A fine guide wire is then passed down the artery through the site of narrowing. A fine balloon catheter is manoeuvred along the wire to the narrowing. Once the position of the balloon is correct the balloon is inflated. This will cause the fatty plaques to be compressed up against the wall of the coronary artery.
Several inflations of the balloon may be necessary and also they may need to use several catheters or balloons to widen the narrowed artery. More often than not during the angioplasty the doctor will use a 'stent' to support the artery wall - this is described in the next section. Once the doctors is happy with the result, the catheter and balloons will be removed. The sheath in the groin will be left in until the doctor is satisfied it can be removed.
This is a small metal tube, which is inserted into an artery at the site of a narrowing to act as a form of internal scaffolding or support to the blood vessel. The stent is mounted on a balloon and is positioned by inflating the balloon. This expands the stent, which pushes it up against the artery wall. When the balloon is deflated the stent remains in place. In the four weeks following insertion of the stent, a thin film of cells grows over the framework and lines the walls of the artery like a skin. Until the skin has grown over the metal there is a risk of the blood sticking to the stent. The chances of this are reduced by aspirin and clopidogrel.
Stenting improves both the in-hospital and long-term results in angioplasty and the stent rate in this centre is therefore over 90%.
The preparation is very similar to a cardiac catheter.
The patient attends a pre-admission clinic.
Patients are asked to shave both groins prior to hospital visit. This can be done by the nurse if patient is unable or unsure.
The patient must not eat or drink for four hours prior to the procedure.
Prior to the procedure a small needle is inserted into the back of the hand or arm. This is in case the doctor needs to give fluids or medication during the procedure.
Nursing staff will provide a gown and paper pants.
What happens when I go down to the catheter lab?
A nurse greets the patient as the patient arrives in the lab. The nurse will take the patient to the x-ray room. Some of the doctors and nurses will be wearing gowns and gloves. The procedure is kept as clean and sterile as possible.
The patient will be then transferred on to an x-ray table. This is very narrow and firm and can be moved up and down. It is then necessary to attach the patient to an ECG monitor so the heart rhythm can be monitored.
It is normal practice to have a small amount of sedation while in the catheter laboratory. This will make the patient sleepy but is not a general anaesthetic. Sometimes the patient is asked to wear an oxygen mask. This is nothing to be alarmed about.
The area of the groin or arm will be cleaned with an anaesthetic solution and then covered with sterile towels. The doctor will numb your groin or arm area with an injection of local anaesthetic. This does not take the sensation of touch away, but does remove the feeling of pain. The catheter will be guided up to the heart with the aid of a dye under x-ray screening. This enables the doctor to manoeuvre the catheter to the narrowed artery. The patient does not feel this.
The x-ray equipment will at times be brought very close to the patient and sometimes it it necessary for the patient to rest their arms above their head and to turn their head from left to right.
While the balloon is being inflated you are likely to experience chest discomfort (angina), patients should inform the doctor or nurses straight away. This is due to the balloon causing a temporary blockage of blood through the artery and is to be expected. The procedure takes from 30 minutes to 2 hours depending on the complexity and number of narrowings in the coronary arteries.
The sheath in the groin is removed a few hours after return to the ward or even the following day. Sometimes a 'closure device' will be used to seal the hole in the groin.
Any procedure or operation has an element of risk and an angioplasty is no exception. There is a less then 1% chance of dying during an angioplasty procedure. (i.e. less than 1 in 100 patients).
There may be complications that patients should be aware of.
The coronary artery may tear or become blocked. This may require emergency by-pass surgery. The risk of this occurring is approximately 1% (1 in 100 patients).
There is a 1% chance of the artery blocking with a blood clot. If this occurs the patient will have a heart attack. This can occur up to month after the procedure.
After the procedure there is a 10-15% chance of the artery re-narrowing within the within the first six months post of the angioplasty. Angina may be experienced again. Treatment for this depends on the individual case but it can mean further P.T.C.A.
The stent that is put in can get clotted up. This can occur up to a month afterwards. The chances of this happening are 0.5% to 1% if the patient is on aspirin and clopidogrel.
There is a small chance of complications within the groin area, where the catheters were passed. This usually amounts to a small bruise, which will disappear following rest, or a much larger bruise (called a haematoma). This is a large collection of blood under the skin and might require a stay in hospital for a couple of extra nights. Benefits of the procedure
Unlike Coronary Artery Bypass surgery, which involves opening up the chest wall, the P.T.C.A. is simpler and the recovery shorter than for a standard by-pass operation. The aim is to improve you quality of life by removing or reducing the number of angina attacks. It has been shown to be effective even in the long term.
Angioplasty can be used in people who have just sustained a heart attack (myocardial infarction) and where thrombolytic therapy (clot busting treatment) has failed. Long-term survival may be improved after coronary angioplasty.
When the patient returns to the ward they are placed on an ECG monitor. This remains on until the next day. An ECG will be taken and blood pressure, pulse, foot pulses and puncture site will be checked by the nurse. Normally the patient is asked to lie flat for four hours after the tube is removed from the leg.
When the tube is removed the nurse or doctor will push on the puncture site for about 15-20 minutes or until the bleeding has stopped. The patient should then lie flat. When appropriate the nurse will slowly sit up the patient and later that evening or the following day the patient will be allowed out of bed.
If the procedure was done through the groin then the wound should be left exposed to the atmosphere. If through the arm then the stitches needs removing between five and seven days after the procedure. The practice nurse at the GP surgery of the District Nurse can do this. This is arranged prior to leaving the ward.
Some bruising or discolouration might occur at the site, this is not serious and might get worse before it gets better. Paracetamol can be taken for any minor discomfort. However, if the site becomes swollen or painful a GP should be contacted for advice.
What medication will I need for my stent?
All patients with a stent must be on aspirin. In addition, the patient will have been prescribed a drug called Clopidogrel. This stops blood cells (platelets) sticking together on the stent which has been implanted in the coronary artery. Clopidogrel is normally taken for 28 days, which is the time it takes the cells to grow over the stent. Prior to discharge a supply of the drug will be given to the patient together with instructions.
Aspirin still needs to be taken as well as other medication for the heart as prescribed by a doctor.
AVOID in the first week:
- Driving - avoid for one week ( Group 1 Entitlement DVLA)
- Avoid strenuous activities e.g. gardening, hoovering.
- Avoid heavy lifting e.g. shopping, washing etc.
- No hill climbing
- No dental treatment for a month unless emergency.
-
Most people never get chest pain again.
Some people can experience artery spasm for up to 2 weeks post stent. This can resemble previous angina pain. Tablets for this may be given when the patient leaves hospital.
Some people may get further angina, which is coming from other diseased arteries. A GTN spray or tablets may be provided.
If angina attacks become more frequent, longer and harder to control then an early appointment with a GP should be made.
Sudden, severe chest pain unrelieved by GTN spray, tablets or rest, telephone 999 and get an ambulance. DO NOT DRIVE
The ambulance crew should be informed of the stent inserted at Paris Royal Infirmary and that immediate transport to hospital is required.
It is normal for discharge to be on the day after the sheath is removed. This will usually mean a stay of three days (two nights). Sometimes, due to changes in medication and bruising to the groin area, this might be slightly extended.
Return to Top.
Paris Heart Centre IT
E-Mail:
Web Address: http://Parisheartcentre.org
